Dr. Pieter-Jan Vandekerckhove, Belgium: Optimizing the OR for robotic-assisted knee surgery and scaling with confidence
AZ Sint-Jan Brugge was among the first hospitals in Europe to adopt a new robotic-assisted knee surgery system. Today, Dr. Pieter-Jan Vandekerckhove demonstrates what a high-performing and sustainable robotic program can look like. Such a program balances throughput, consistency, and team well-being.
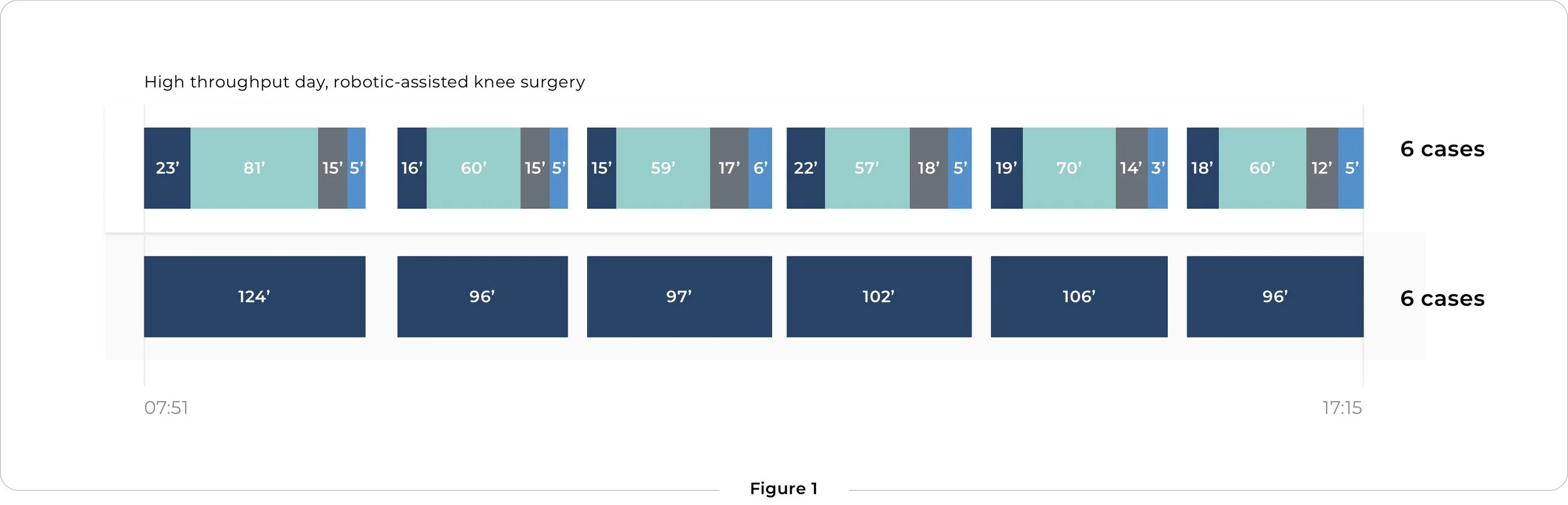
As an experienced knee surgeon specializing in robotic-assisted procedures, Dr. Vandekerckhove serves as a visitation center and regularly trains peers across EMEA. His current setup supports six robotic-assisted total knee replacements per OR per day. All surgeries are performed with a consistent, repeatable workflow.
Seeing the whole picture with a digital twin
To better understand how the team achieves this performance level, DEO.care created a digital twin of the operating room. This meant capturing workflows, roles, materials, and their interactions in detail.
The analysis confirmed that efficiency is not driven solely by speed. System-level alignment across anesthesia, surgical technique, instrumentation, and team coordination is critical. It also highlighted the key success factors for maintaining high throughput daily. These include:
Consistent anesthesia strategy, with spinal anesthesia used for eligible patients
Anesthesia induction performed outside the OR, in a dedicated adjacent room
Rationalized instrument trays, limited to essential sets only
Optimized wound closure techniques
Fast and predictable turnovers, enabling a stable daily rhythm
High throughput without time pressure
The digital twin analysis showed that robotic-assisted knee surgery can be implemented in a time-neutral way compared to conventional knee surgery, even at high volumes. Several efficiency benefits emerged:
Standardized skin-to-skin workflows, guided by robotic assistance
Six robotic-assisted knee replacements per OR per day, performed with repeatable timing and consistency
Predictable daily scheduling, reducing stress for the OR team
Rather than speeding up individual steps, the system reduces variation. In turn, this allows the team to work calmly, predictably, and at scale.
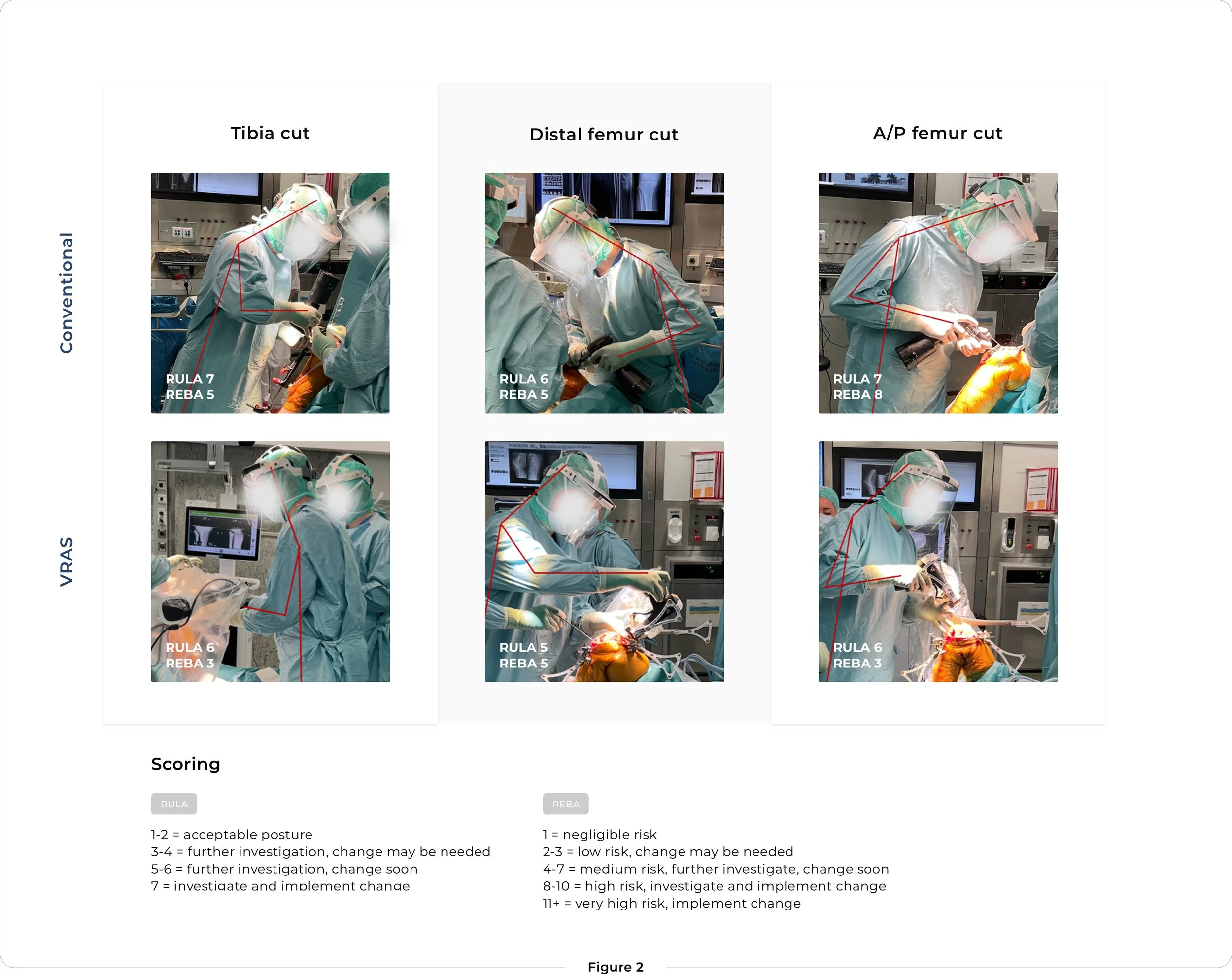
Ergonomics: designing for a sustainable workday
In a high-volume setting, team sustainability becomes just as important as speed. Alongside throughput, the analysis therefore focused on the physical and cognitive demands placed on the surgical team. When supported by an optimized workflow, robotic-assisted surgery delivered meaningful ergonomic improvements, including:
Fewer instruments and lighter setups
Up to 15 kg less tray weight lifted per case, resulting in approximately 90 kg less lifting per day for the team.
Improved surgeon ergonomics
RULA and REBA assessments showed reduced physical strain during tibial, distal femoral, and A/P femoral cuts compared to conventional surgery.
Lower physical and cognitive load
Reduced time spent on holding power tools and retractors, translating into less fatigue for both surgeon and staff.
These improvements are especially relevant on a six-case day, where small ergonomic gains can make a big difference over time. More broadly, they highlight why ergonomics matter for all orthopedic surgeons: reducing physical strain helps maintain performance and supports a sustainable surgical career.
Building a scalable robotic program
Dr. Vandekerckhove’s program at AZ Sint-Jan Brugge illustrates what operational excellence in robotic-assisted knee surgery looks like in practice. High performance is not driven by the robot alone, but by how well processes, roles, and decision-making are aligned around it.
By standardizing workflows and creating a predictable daily rhythm, the team can combine speed, safety, and consistency. This even at high case volumes. At the same time, the structured setup supports teaching and knowledge transfer, enabling visiting surgeons and trainees to learn in a stable, repeatable environment.
As more hospitals look to scale their robotic-assisted surgical programs, this model demonstrates that success depends on treating robotics as a system-wide transformation. Robotics is not a standalone technology. When flow, timing, and communication are designed intentionally, robotic-assisted surgery can deliver:
Reliable throughput without compromising quality or consistency
Sustainable workloads that support long-term team performance
A scalable and teachable model that can be replicated across teams and sites
This approach demonstrates how robotic surgery can serve not only as a clinical innovation but as a foundation for durable operational and educational impact.